The Connection Between Menopause and Osteoporosis
Catagory: Gynaecology & Obstetricts Author: Dr Rekha Prabhu
As women age, they experience various physical and hormonal changes, one of which is menopause. Menopause is a natural biological process that marks the end of a woman’s reproductive years. It is often associated with a range of symptoms, including hot flashes, mood swings, and changes in bone density. The connection between menopause and osteoporosis, a condition characterized by weakened bones and an increased risk of fractures.
Understanding Menopause:
Menopause typically occurs between the ages of 45 and 55, with the average age being 51. During this stage, a woman’s ovaries gradually produce less estrogen and progesterone, two key hormones involved in the reproductive system. The hormonal fluctuations associated with menopause can have a significant impact on bone health.
The Role of Estrogen:
Estrogen plays a crucial role in maintaining bone density. It helps regulate the process of bone remodeling, which involves the breakdown and formation of bone tissue. Estrogen helps inhibit bone breakdown by reducing the activity of osteoclasts, cells that break down bone tissue. Additionally, estrogen stimulates the production of osteoblasts, cells that help build new bone. Therefore, a decrease in estrogen levels during menopause can lead to a higher rate of bone loss and a higher risk of developing osteoporosis.
Osteoporosis and Bone Health:
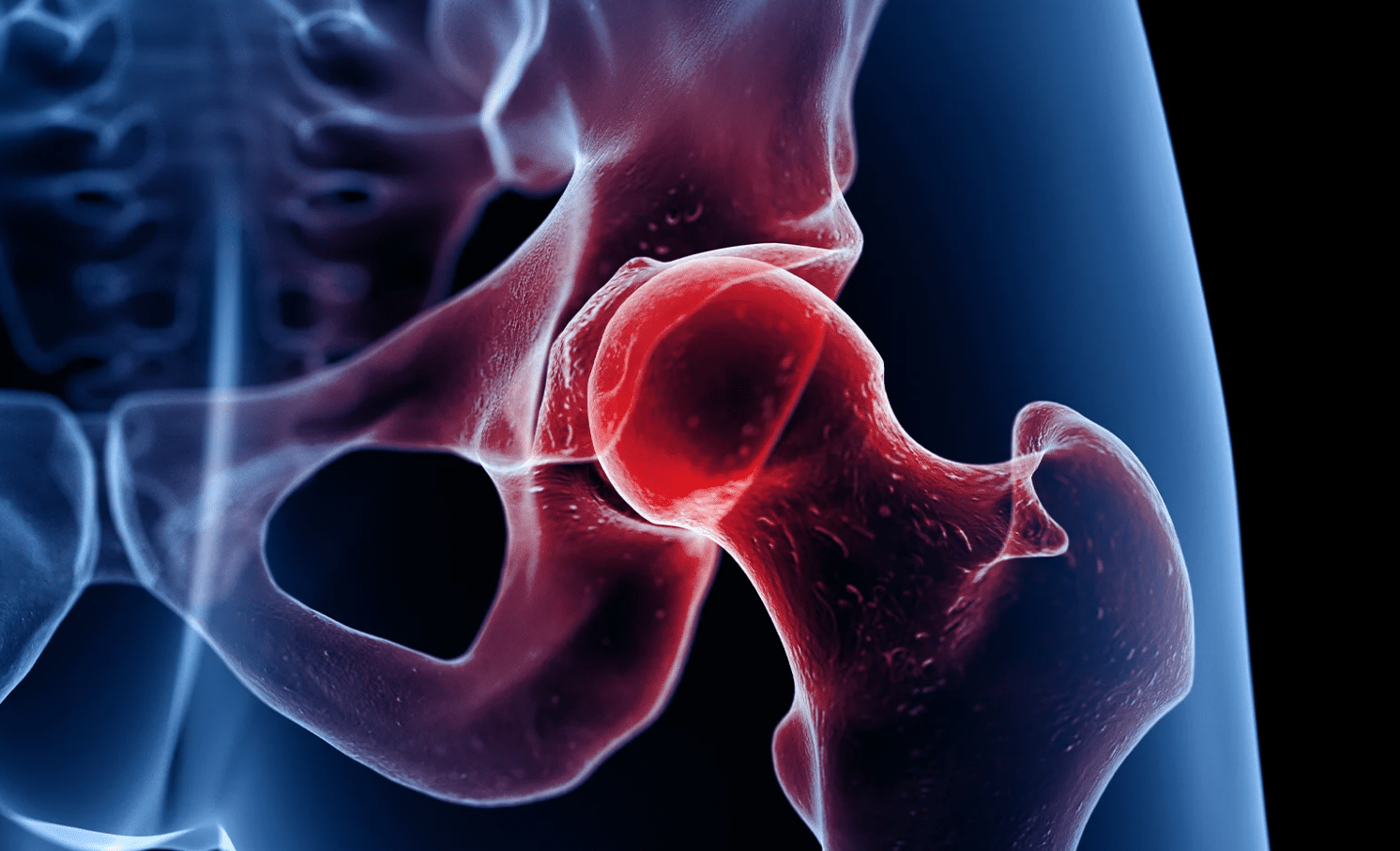
Osteoporosis is a condition characterized by low bone mass and deterioration of bone tissue, leading to increased bone fragility and susceptibility to fractures. Although osteoporosis can affect both men and women, postmenopausal women are at a higher risk due to the hormonal changes they experience.
The hormonal changes during menopause contribute to the development of osteoporosis in several ways. As estrogen levels decline, bone breakdown can exceed bone formation, resulting in a net loss of bone density. This loss of bone density weakens the structure of the bones, making them more prone to fractures, especially in the hips, spine, and wrists.
The Link Between Menopause and Osteoporosis:
The relationship between menopause and osteoporosis is primarily attributed to the decline in estrogen levels. Studies have shown that women can lose up to 20% of their bone density in the first 5-7 years after menopause. The rate of bone loss gradually slows down afterward but continues throughout the postmenopausal years.
Other factors that can influence the development of osteoporosis include:
Age: The risk of osteoporosis increases with age, and the decline in estrogen levels during menopause exacerbates this risk.
Genetics: A family history of osteoporosis or fractures can increase an individual’s susceptibility to the condition.
Lifestyle Factors: Poor nutrition, sedentary lifestyle, smoking, excessive alcohol consumption, and low levels of physical activity can contribute to the development of osteoporosis.
Prevention and Management:
While menopause is an inevitable part of a woman’s life, there are steps that can be taken to prevent or manage osteoporosis:
Calcium and Vitamin D: A diet rich in calcium and vitamin D is crucial for maintaining bone health. Dairy products, leafy green vegetables, fortified cereals, and exposure to sunlight are excellent sources of these nutrients.
Regular Exercise: Engaging in weight-bearing exercises, such as walking, jogging, and resistance training, can help strengthen bones and reduce the risk of fractures.
Lifestyle Modifications: Quitting smoking, limiting alcohol consumption, and maintaining a healthy body weight can positively impact bone health.
Hormone Replacement Therapy (HRT): HRT involves the use of medications containing estrogen and progesterone to relieve menopausal symptoms and minimize bone loss. However, the decision to undergo HRT should be made in consultation with a healthcare professional, considering individual health risks and benefits.
Bone Density Testing: Periodic bone density tests, such as dual-energy X-ray absorptiometry (DEXA), can assess bone strength and identify individuals at higher risk of osteoporosis.
Conclusion
In conclusion, menopause and osteoporosis are intimately connected, primarily due to the hormonal modifications that occur during this stage of a woman’s life. The decline in estrogen levels heightens the risk of bone loss and the onset of osteoporosis. Nevertheless, by implementing preventive measures and embracing a lifestyle that promotes bone health, women can mitigate the risk of osteoporosis and maintain strong bones well into their later years. Regular consultations with healthcare professionals are essential for devising personalized strategies to manage menopause and preserve bone health. And if you’re seeking the best pediatric critical care consultant in Tirupati, our team of highly skilled professionals is ready to provide expert guidance and support for your child’s critical care needs.
Recent Post
-
Transen Sex Aachen Verlockende Begleiterinnen
-
Exclusive Access. Get Your Hands on Young Thug Spider Brands Latest Sale 50% Off
-
Common Gynecological Issues and When to See a Specialist in Vijayawada: Insights
-
Gynecological Health for Teens: Expert Guidance from Vijayawada Specialists
-
Embracing Women's Wellness: The Holistic Path to Reproductive Health
-
Unlocking Gynecological Health: Expert Insights by Dr. Rekha Prabhu
-
From Conception to Delivery: Insights into Pregnancy and Obstetrics
-
Beyond Birth: Navigating Women's Health Throughout Every Stage of Life
-
Yoga for Women’s During Pregnancy
-
Genetic Testing in Gynecological Healthcare
-
Exercises for Pelvic Floor Health
-
Preventing Vaginal Infections and Irritations
-
MONIXBET CASINO ALGEMEEN OVERZICHT
-
Unveiling the Vital Link: Sleep and Women's Health | Dr Rekha Prabhu
-
Exploring the Benefits of Meditation and Yoga for Women's Health
-
Understanding and Managing Common Pregnancy Complications
-
Endometriosis: Diagnosis, Treatment, and Lifestyle Management
-
The Connection Between Diabetes and Pregnancy
-
What You Need to Know About Uterine Fibroids
-
The Connection Between Menopause and Osteoporosis
